How to Teach a Breastfeeding Class: Important Discussions & Fun Activities
Quote from Jessa VonFeldt on March 7, 2024, 9:03 amWritten by Debbie Young, MSL, ICCE, LCCE, CLC
I recently worked with a new mom and her slightly early baby. After the lengthy birth, the baby was put to Mom’s chest and within the hour they were nursing happily, and by the time I left that evening, things seemed to be going very well. By the time I visited again the next day, things were not as idyllic. The lactation consultant had been in the next morning, but it was difficult for the mother to wake up enough to ask questions or respond. Later that day, another lactation consultant came in, but the mother did not feel she got the information that helped. She felt she got a rote answer to her specific breast pain instead of having the consultant ask for more info. She said the best information she got was from an IBCLC who was orienting as a new mom/baby nurse on the postpartum unit. The nurse took time to listen to the new mother and helped her think about ways to make breastfeeding work for her.
Some new mothers, like this one, will eventually find the right person to help in the hospital, but without some prenatal education about breastfeeding, it may be harder to get started on the right foot. Or, for some families, there may be no one during the early time at home who has knowledge about breastfeeding. The CDC latest data depicts breastfeeding drops approximately 30% by three months1. This may be planned by the parents, or it may show that without enough education and support, it is difficult to breastfeed. Many new parents may have never experienced seeing others with newborns or older babies breastfeed.
So, how can we help families understand the benefits and commit to continuing breastfeeding for the long run? Education and support are the dual strategies to make this happen. Prenatally, parents can learn about breastfeeding while they are more aware and alert than they will be right after birth. Beyond childbirth education classes, which may cover breastfeeding briefly, specific prenatal breastfeeding classes will help parents succeed in this area of their new-parent journey. Successful initiation and length of duration may be enhanced by having a prenatal class specifically devoted to breastfeeding.
I’ve taught breastfeeding classes for many years in both hospital and private settings. It might seem overwhelming to set one up, but it can be made easier with the right resources. I like using a PowerPoint with embedded videos. I also use a book for parents to take home that corresponds to the PowerPoint, as well as different props to engage students. Having baby dolls and a breast model on hand is helpful. Read on to for some specific tips for running a new class or integrating fresh ideas into an existing class.
Engaging parents from the first step into your classroom
Before class, I put the student workbook and one plastic spoon on each table. Each plastic spoon will have one of three marbles in it. One will be the typical small marble, another table’s spoon will have a “shooter” marble, and the other option will be a large marble about the size of a ping pong ball on the spoon. After we go over the agenda, we introduce ourselves. I ask the learners to tell if they were breastfed or have ever seen someone breastfeed. It is an eye-opening discussion! Then we move on to looking at the items on the desks. I explain that the book is great reference material that I may refer to during class and that they can take home for later. I point out that it also has a web app with some of the video content from the class, along with other great parent resources.
Next, I ask what they think the spoon and marble are all about. We guess the volume that could fit into a small marble, which is the size of a newborn baby’s stomach. Then, we do the same for the shooter marble (which shows the one-week-old stomach) and finally the ping pong sized marble (which shows the two-week-old newborn’s stomach). I also hold up a 1- and 2-ounce bottle and put the smallest and middle-sized marble in them, respectively, to help them understand the small amount the baby will take at each nursing time to begin with. This also helps as a visual if mom will be pumping and thinking she is not getting enough. We also talk about a baby taking the amount of milk that fills their stomach but not more. This is a great time to talk about how efficient the baby’s body is at breaking down and using breastmilk quickly—and stressing that nursing 8-12 times in 24 hours is important for newborns.
One of the things that parents cling to that they’ve heard from other sources is to breastfeed “every 2 to 3 hours,” because that feels predictable and manageable. To dispel this idea, I break the class up into 2 groups and give each group some beads and string and invite them to portray what that will look like using the beads. The first tries are predictably well spaced, with the beads in equal intervals on the string. Then, we talk about cluster feeding in the first couple of nights and in later growth phases. We demonstrate what that looks like using the beads and string. I always let them know that they may feel a bit discombobulated as they watch the baby instead of the clock, but to feel assured knowing their newborn won’t overfeed. My mantra I suggest for them is, “You learn from the baby first, then you teach the baby later other important life skills.”
Positive health outcomes for children and women/breastfeeding parents
Next, using the PowerPoint slides with the videos, we explore the benefits of breastfeeding for their newborn. Babies are less likely to have ear infections and stomach bugs and may be protected from other communicable diseases. Because babies get antibodies from their mother’s milk, they build a stronger immune system, and this can protect them from other illnesses. They also have a lower risk of developing asthma, obesity, type 1 diabetes and dying of SIDS3.
Then we move on to the women. The mother gets health benefits too. Women who breastfeed have a lower risk of breast cancer, ovarian cancer, high blood pressure and type 2 diabetes2. This information is significant, and through discussion everyone in the class may agree that it makes sense to initiate breastfeeding for these benefits. But we also need to encourage parents to continue with their plan to breastfeed, even if things are not ideal at birth. We discuss that if either the mother or baby has extra medical issues, continuing with the plan to breastfeed and/or use breastmilk should be pursued by touching on the benefits of breastmilk to sick or premature infants. Mothers who have many of the risk factors for morbidity and mortality, including major coronary events, later in their life can use breastfeeding to lower their risks. Heart disease is the leading cause of death for women in the US. Breastfeeding improves cardiovascular health, it gives cardioprotective effects of oxytocin and helps the mother long term.
How breastfeeding works
In the PowerPoint I use, we watch a video animation of how the body creates and gives the baby access to the milk through nursing. It is such an “ah-ha” moment for most students. (I often get a specific mention of that in the class evaluations.) During this part of the class, we also discuss other things like the changing nature of the milk in the first few days from colostrum to mature milk. One student said that her online mama’s group was talking about the “fact” that there is no milk until close to the end of the first week, and she wondered what to feed the baby before then. It was a great discussion about how colostrum is the first milk and that it’s power packed with immune-building properties, as well as being a great source of nutrients and substances that help build the baby’s guts with good bacteria.
How to breastfeed
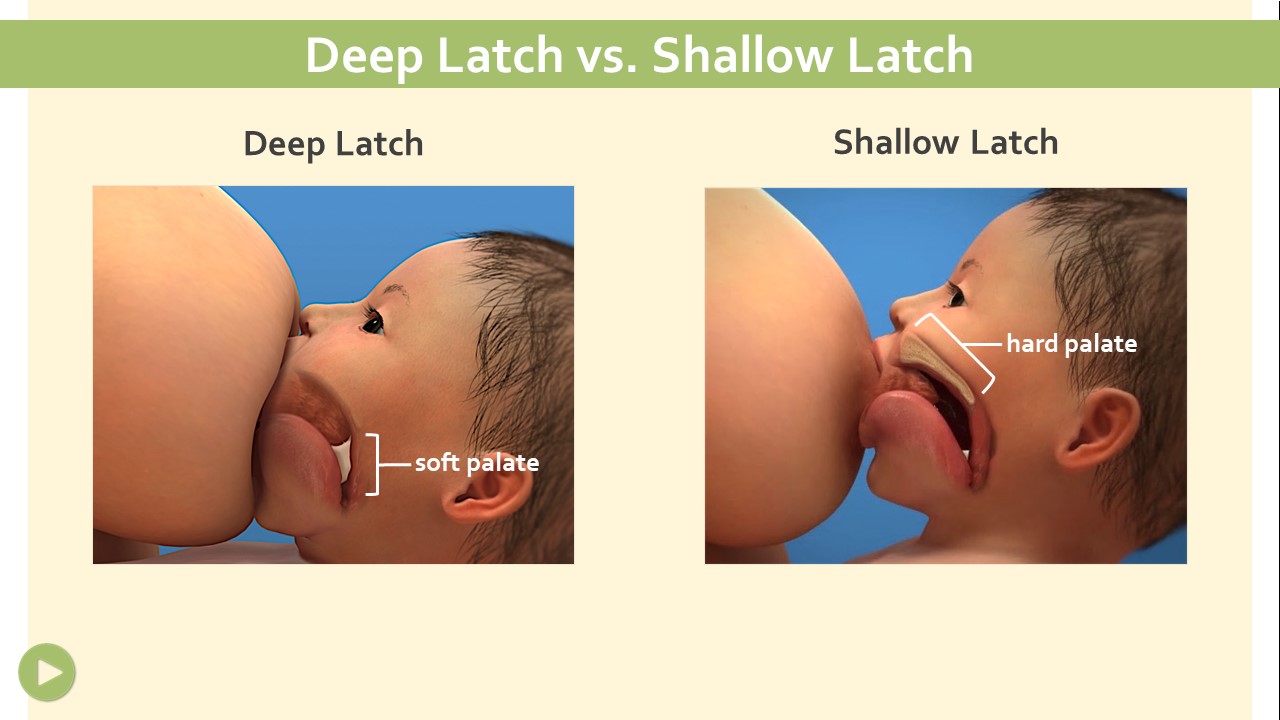
After covering how the breast makes milk, we now talk about the “delivery system.” Using a knitted breast model, we discuss the areola and nipple. It is helpful for me to use my hand as the baby’s mouth and apply it to the breast model in various ways, showing good and ineffective latches. We watch another video showing good and poor latches (both using animation to see what is happening from the inside and using live footage) so parents can see this up close and personally. We talk about the difference between breastfeeding (with a good amount of the tissue surrounding the nipple in their mouth) and nipple feeding (just taking the nipple), which decreases the amount of milk baby gets and causes sore and possibly damaged nipples. We discuss the methods for helping baby open wide with nipple to nose. With my model baby doll, I use my knitted breast and position the baby on the breast with a nipple to nose position. Then I set the doll aside and use my hand with the middle knuckle standing for the nose aligned with the nipple on the breast model. I show how the chin (bottom of my hand) connects with the lower part of the breast and then open my hand to take in the proper amount of tissue for a successful latch.
We then view a video about positioning the baby for successful breastfeeding. I have five dolls I use for demonstrations, but I invite students to bring in their own a baby sized doll or stuffed animal in a pre-class email. Depending on the number of students in the class, I give each one a baby doll, if needed, or they split into small groups, each group getting one doll. Then, we practice various positions and discuss the potential for feeling awkward and ways to support mom’s body and the baby to feel comfortable. Using my breast model and a baby, I position incorrectly and ask the group to explain how to move myself or the baby to get a better latch. This helps build critical thinking.
When to feed your baby
Next, I refer to the earlier activity about how often to feed the baby and provide information on trusting the baby to show hunger cues. If the baby is missing that “8 to 12 times per 24 hour” schedule then we talk about making sure to wake the baby to feed when they’re in light sleep. I show what the deep and active sleep cycles look like on my doll. To show a baby in deep sleep, I place the doll face up on the table and I pick up the arm and it flops back down instantly. Then we talk about a baby in a lighter sleep phase moving, eyes fluttering, possibly showing feeding cues. I encourage them to catch the baby in light sleep if possible so the baby isn’t too sleepy to feed effectively.
Assuring baby is getting enough milk
One of the top reasons parents quit breastfeeding is a fear that the baby is not getting enough milk. Besides pumping and feeding a bottle, there is no good way to measure the amount of breastmilk going in. This is a big fear, so many new parents consider formula feeding (or even pumping and feeding) as a way to mitigate that concern. Throughout my class discussions, I hope to instill confidence that the baby and the breast know how much milk is needed and the symbiotic relationship between the two means the baby is getting the right amount of milk. I let them know that baby’s weight gain can also assure them of this and that many lactation consultants will have a scale available. But the biggest tip I give for when they are home is to pay attention to the number and look of wet and dirty diapers. I have a slide on my presentation that shows the averages and when to seek help. We discuss color, texture, and number of bowel movements and how they change over time.
Involving the father/partner for success
One client I was working with told me she didn’t think she would have continued to breastfeed without the encouragement and knowledge that her husband had gained during the breastfeeding class. Be sure you include the partners in the discussions, critical thinking, and all parts of the class. Burping seems to be a special place where some like to become experts. One dad, who was already a father, had a new partner and gave some good tips to the other dads. He mentioned that when the baby woke at night he would check to see if the diaper needed changing before giving the baby to the mother. He mentioned that he kept a fresh supply of water on the table next to her favorite nursing chair. He also encouraged her to nurse wherever they were without regard to what others around them thought. I could see other dads shaking their heads in agreement.
Breastfeeding lifestyles
We end the class by talking about how to feel confident nursing wherever the baby is hungry, no matter where you are. I have a couple of capes, showing how they can cover up if desired, but stress that all 50 states allow breastfeeding with or without coverings now. I give a couple of examples of people who stood up for their rights to breastfeed in an out-of-home environment. We also talk about pumping because 85% of women pump at least sometimes, and 6% exclusively pump4. I have a pump and the paraphernalia that goes with it. We look at how pumps generally work. I mention that many insurance companies will also pay for a pump and even visits with a lactation consultant. If they want to know more, they can contact their insurance company. We also talk about laws that dictate that most businesses must give time and set up an area for pumping that is not the bathroom.
The positive class evaluations I receive and stories of success I hear later make me happy to help parents get off to the best start when breastfeeding. The parents also leave with a schedule of the local mom/baby group on Mondays and family group meetings on alternate Thursday evenings. I tell them that meeting with others that are breastfeeding can be very helpful.
1Breastfeeding Report Card, United States, 2022
3Breastfeeding Benefits Both Baby and Mom (2023)
4Pumping Milk and Nursing Are Not the Same, Lowery, A, (2019) https://www.theatlantic.com/ideas/archive/2019/07/exclusive-pumping-research/594580/ “Jill Lepore’s evocative phrasing, their own wet nurses”
InJoy Resources:
Understanding Breastfeeding Book + Web App
Understanding Breastfeeding PowerPoint Class
Understanding Breastfeeding Video Program
Debbie Young, MSL, ICCE, LCCE, CLC, ICBD, is the Customer Relations Manager at InJoy. Working with families as an educator and doula for over 30 years and after using InJoy products in her work since 1994, Debbie joined the InJoy team in 2013. She continues to be involved with families as a doula and a childbirth educator on a part-time basis. She teaches, writes and speaks on various birth, postpartum and building family subjects. Debbie is a past president of DONA International and was the Managing Editor for the International Doula for eight years. She is the current President of ICEA. She has a BA in Health Promotion: Women’s Health and a Master’s in Leadership through Grand Canyon University. Debbie has interviewed many leading professionals in the Maternal/Child field.
Written by Debbie Young, MSL, ICCE, LCCE, CLC
 I recently worked with a new mom and her slightly early baby. After the lengthy birth, the baby was put to Mom’s chest and within the hour they were nursing happily, and by the time I left that evening, things seemed to be going very well. By the time I visited again the next day, things were not as idyllic. The lactation consultant had been in the next morning, but it was difficult for the mother to wake up enough to ask questions or respond. Later that day, another lactation consultant came in, but the mother did not feel she got the information that helped. She felt she got a rote answer to her specific breast pain instead of having the consultant ask for more info. She said the best information she got was from an IBCLC who was orienting as a new mom/baby nurse on the postpartum unit. The nurse took time to listen to the new mother and helped her think about ways to make breastfeeding work for her.
I recently worked with a new mom and her slightly early baby. After the lengthy birth, the baby was put to Mom’s chest and within the hour they were nursing happily, and by the time I left that evening, things seemed to be going very well. By the time I visited again the next day, things were not as idyllic. The lactation consultant had been in the next morning, but it was difficult for the mother to wake up enough to ask questions or respond. Later that day, another lactation consultant came in, but the mother did not feel she got the information that helped. She felt she got a rote answer to her specific breast pain instead of having the consultant ask for more info. She said the best information she got was from an IBCLC who was orienting as a new mom/baby nurse on the postpartum unit. The nurse took time to listen to the new mother and helped her think about ways to make breastfeeding work for her.
Some new mothers, like this one, will eventually find the right person to help in the hospital, but without some prenatal education about breastfeeding, it may be harder to get started on the right foot. Or, for some families, there may be no one during the early time at home who has knowledge about breastfeeding. The CDC latest data depicts breastfeeding drops approximately 30% by three months1. This may be planned by the parents, or it may show that without enough education and support, it is difficult to breastfeed. Many new parents may have never experienced seeing others with newborns or older babies breastfeed.
So, how can we help families understand the benefits and commit to continuing breastfeeding for the long run? Education and support are the dual strategies to make this happen. Prenatally, parents can learn about breastfeeding while they are more aware and alert than they will be right after birth. Beyond childbirth education classes, which may cover breastfeeding briefly, specific prenatal breastfeeding classes will help parents succeed in this area of their new-parent journey. Successful initiation and length of duration may be enhanced by having a prenatal class specifically devoted to breastfeeding.
 I’ve taught breastfeeding classes for many years in both hospital and private settings. It might seem overwhelming to set one up, but it can be made easier with the right resources. I like using a PowerPoint with embedded videos. I also use a book for parents to take home that corresponds to the PowerPoint, as well as different props to engage students. Having baby dolls and a breast model on hand is helpful. Read on to for some specific tips for running a new class or integrating fresh ideas into an existing class.
I’ve taught breastfeeding classes for many years in both hospital and private settings. It might seem overwhelming to set one up, but it can be made easier with the right resources. I like using a PowerPoint with embedded videos. I also use a book for parents to take home that corresponds to the PowerPoint, as well as different props to engage students. Having baby dolls and a breast model on hand is helpful. Read on to for some specific tips for running a new class or integrating fresh ideas into an existing class.
Engaging parents from the first step into your classroom
Before class, I put the student workbook and one plastic spoon on each table. Each plastic spoon will have one of three marbles in it. One will be the typical small marble, another table’s spoon will have a “shooter” marble, and the other option will be a large marble about the size of a ping pong ball on the spoon. After we go over the agenda, we introduce ourselves. I ask the learners to tell if they were breastfed or have ever seen someone breastfeed. It is an eye-opening discussion! Then we move on to looking at the items on the desks. I explain that the book is great reference material that I may refer to during class and that they can take home for later. I point out that it also has a web app with some of the video content from the class, along with other great parent resources.

Next, I ask what they think the spoon and marble are all about. We guess the volume that could fit into a small marble, which is the size of a newborn baby’s stomach. Then, we do the same for the shooter marble (which shows the one-week-old stomach) and finally the ping pong sized marble (which shows the two-week-old newborn’s stomach). I also hold up a 1- and 2-ounce bottle and put the smallest and middle-sized marble in them, respectively, to help them understand the small amount the baby will take at each nursing time to begin with. This also helps as a visual if mom will be pumping and thinking she is not getting enough. We also talk about a baby taking the amount of milk that fills their stomach but not more. This is a great time to talk about how efficient the baby’s body is at breaking down and using breastmilk quickly—and stressing that nursing 8-12 times in 24 hours is important for newborns.
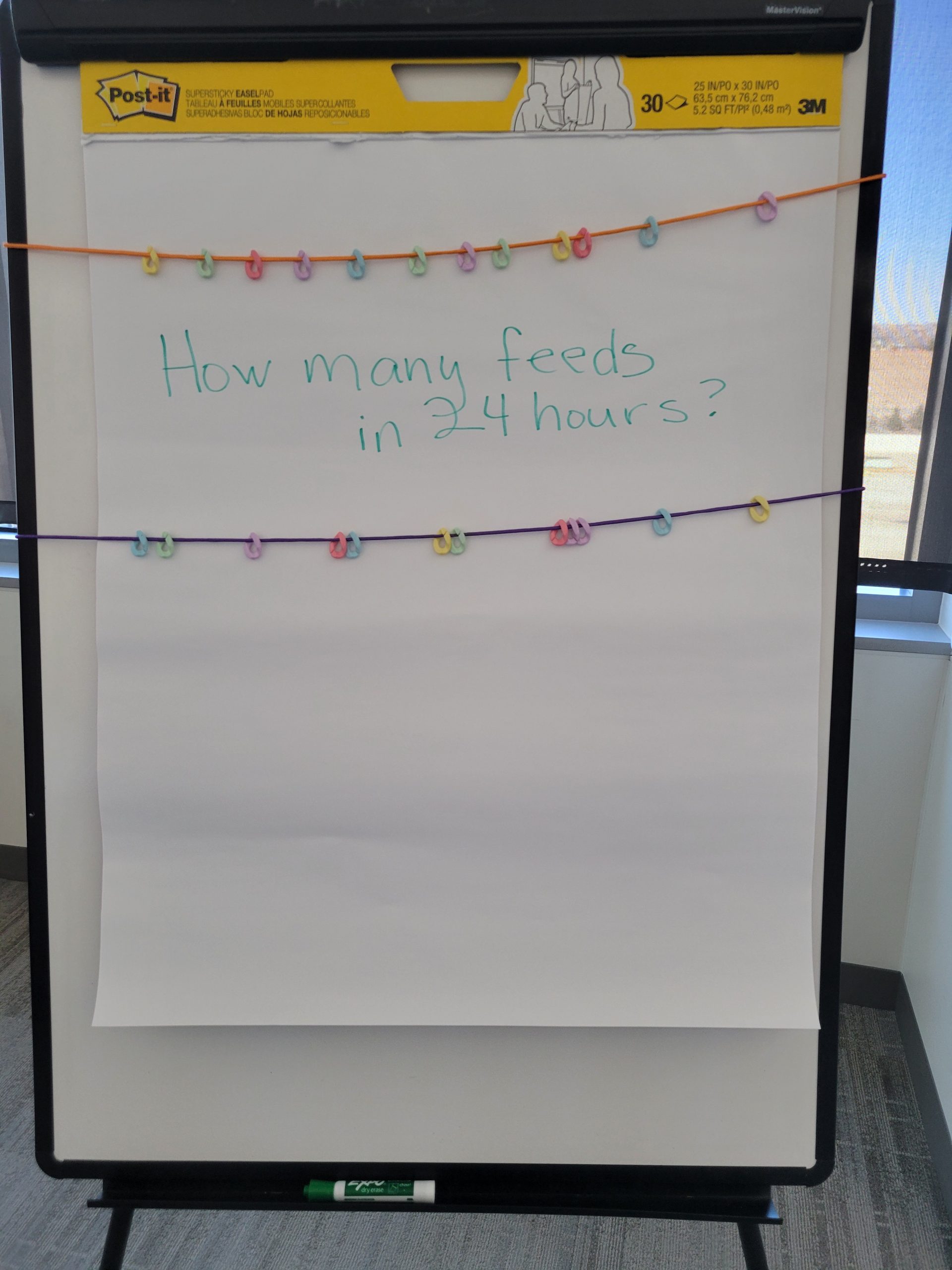 One of the things that parents cling to that they’ve heard from other sources is to breastfeed “every 2 to 3 hours,” because that feels predictable and manageable. To dispel this idea, I break the class up into 2 groups and give each group some beads and string and invite them to portray what that will look like using the beads. The first tries are predictably well spaced, with the beads in equal intervals on the string. Then, we talk about cluster feeding in the first couple of nights and in later growth phases. We demonstrate what that looks like using the beads and string. I always let them know that they may feel a bit discombobulated as they watch the baby instead of the clock, but to feel assured knowing their newborn won’t overfeed. My mantra I suggest for them is, “You learn from the baby first, then you teach the baby later other important life skills.”
One of the things that parents cling to that they’ve heard from other sources is to breastfeed “every 2 to 3 hours,” because that feels predictable and manageable. To dispel this idea, I break the class up into 2 groups and give each group some beads and string and invite them to portray what that will look like using the beads. The first tries are predictably well spaced, with the beads in equal intervals on the string. Then, we talk about cluster feeding in the first couple of nights and in later growth phases. We demonstrate what that looks like using the beads and string. I always let them know that they may feel a bit discombobulated as they watch the baby instead of the clock, but to feel assured knowing their newborn won’t overfeed. My mantra I suggest for them is, “You learn from the baby first, then you teach the baby later other important life skills.”
Positive health outcomes for children and women/breastfeeding parents
Next, using the PowerPoint slides with the videos, we explore the benefits of breastfeeding for their newborn. Babies are less likely to have ear infections and stomach bugs and may be protected from other communicable diseases. Because babies get antibodies from their mother’s milk, they build a stronger immune system, and this can protect them from other illnesses. They also have a lower risk of developing asthma, obesity, type 1 diabetes and dying of SIDS3.
Then we move on to the women. The mother gets health benefits too. Women who breastfeed have a lower risk of breast cancer, ovarian cancer, high blood pressure and type 2 diabetes2. This information is significant, and through discussion everyone in the class may agree that it makes sense to initiate breastfeeding for these benefits. But we also need to encourage parents to continue with their plan to breastfeed, even if things are not ideal at birth. We discuss that if either the mother or baby has extra medical issues, continuing with the plan to breastfeed and/or use breastmilk should be pursued by touching on the benefits of breastmilk to sick or premature infants. Mothers who have many of the risk factors for morbidity and mortality, including major coronary events, later in their life can use breastfeeding to lower their risks. Heart disease is the leading cause of death for women in the US. Breastfeeding improves cardiovascular health, it gives cardioprotective effects of oxytocin and helps the mother long term.
How breastfeeding works
In the PowerPoint I use, we watch a video animation of how the body creates and gives the baby access to the milk through nursing. It is such an “ah-ha” moment for most students. (I often get a specific mention of that in the class evaluations.) During this part of the class, we also discuss other things like the changing nature of the milk in the first few days from colostrum to mature milk. One student said that her online mama’s group was talking about the “fact” that there is no milk until close to the end of the first week, and she wondered what to feed the baby before then. It was a great discussion about how colostrum is the first milk and that it’s power packed with immune-building properties, as well as being a great source of nutrients and substances that help build the baby’s guts with good bacteria.
How to breastfeed
After covering how the breast makes milk, we now talk about the “delivery system.” Using a knitted breast model, we discuss the areola and nipple. It is helpful for me to use my hand as the baby’s mouth and apply it to the breast model in various ways, showing good and ineffective latches. We watch another video showing good and poor latches (both using animation to see what is happening from the inside and using live footage) so parents can see this up close and personally. We talk about the difference between breastfeeding (with a good amount of the tissue surrounding the nipple in their mouth) and nipple feeding (just taking the nipple), which decreases the amount of milk baby gets and causes sore and possibly damaged nipples. We discuss the methods for helping baby open wide with nipple to nose. With my model baby doll, I use my knitted breast and position the baby on the breast with a nipple to nose position. Then I set the doll aside and use my hand with the middle knuckle standing for the nose aligned with the nipple on the breast model. I show how the chin (bottom of my hand) connects with the lower part of the breast and then open my hand to take in the proper amount of tissue for a successful latch.
We then view a video about positioning the baby for successful breastfeeding. I have five dolls I use for demonstrations, but I invite students to bring in their own a baby sized doll or stuffed animal in a pre-class email. Depending on the number of students in the class, I give each one a baby doll, if needed, or they split into small groups, each group getting one doll. Then, we practice various positions and discuss the potential for feeling awkward and ways to support mom’s body and the baby to feel comfortable. Using my breast model and a baby, I position incorrectly and ask the group to explain how to move myself or the baby to get a better latch. This helps build critical thinking.
When to feed your baby
Next, I refer to the earlier activity about how often to feed the baby and provide information on trusting the baby to show hunger cues. If the baby is missing that “8 to 12 times per 24 hour” schedule then we talk about making sure to wake the baby to feed when they’re in light sleep. I show what the deep and active sleep cycles look like on my doll. To show a baby in deep sleep, I place the doll face up on the table and I pick up the arm and it flops back down instantly. Then we talk about a baby in a lighter sleep phase moving, eyes fluttering, possibly showing feeding cues. I encourage them to catch the baby in light sleep if possible so the baby isn’t too sleepy to feed effectively.
Assuring baby is getting enough milk
One of the top reasons parents quit breastfeeding is a fear that the baby is not getting enough milk. Besides pumping and feeding a bottle, there is no good way to measure the amount of breastmilk going in. This is a big fear, so many new parents consider formula feeding (or even pumping and feeding) as a way to mitigate that concern. Throughout my class discussions, I hope to instill confidence that the baby and the breast know how much milk is needed and the symbiotic relationship between the two means the baby is getting the right amount of milk. I let them know that baby’s weight gain can also assure them of this and that many lactation consultants will have a scale available. But the biggest tip I give for when they are home is to pay attention to the number and look of wet and dirty diapers. I have a slide on my presentation that shows the averages and when to seek help. We discuss color, texture, and number of bowel movements and how they change over time.
 Involving the father/partner for success
Involving the father/partner for success
One client I was working with told me she didn’t think she would have continued to breastfeed without the encouragement and knowledge that her husband had gained during the breastfeeding class. Be sure you include the partners in the discussions, critical thinking, and all parts of the class. Burping seems to be a special place where some like to become experts. One dad, who was already a father, had a new partner and gave some good tips to the other dads. He mentioned that when the baby woke at night he would check to see if the diaper needed changing before giving the baby to the mother. He mentioned that he kept a fresh supply of water on the table next to her favorite nursing chair. He also encouraged her to nurse wherever they were without regard to what others around them thought. I could see other dads shaking their heads in agreement.
Breastfeeding lifestyles
We end the class by talking about how to feel confident nursing wherever the baby is hungry, no matter where you are. I have a couple of capes, showing how they can cover up if desired, but stress that all 50 states allow breastfeeding with or without coverings now. I give a couple of examples of people who stood up for their rights to breastfeed in an out-of-home environment. We also talk about pumping because 85% of women pump at least sometimes, and 6% exclusively pump4. I have a pump and the paraphernalia that goes with it. We look at how pumps generally work. I mention that many insurance companies will also pay for a pump and even visits with a lactation consultant. If they want to know more, they can contact their insurance company. We also talk about laws that dictate that most businesses must give time and set up an area for pumping that is not the bathroom.
The positive class evaluations I receive and stories of success I hear later make me happy to help parents get off to the best start when breastfeeding. The parents also leave with a schedule of the local mom/baby group on Mondays and family group meetings on alternate Thursday evenings. I tell them that meeting with others that are breastfeeding can be very helpful.
1Breastfeeding Report Card, United States, 2022
3Breastfeeding Benefits Both Baby and Mom (2023)
4Pumping Milk and Nursing Are Not the Same, Lowery, A, (2019) https://www.theatlantic.com/ideas/archive/2019/07/exclusive-pumping-research/594580/ “Jill Lepore’s evocative phrasing, their own wet nurses”
InJoy Resources:
Understanding Breastfeeding Book + Web App
Understanding Breastfeeding PowerPoint Class
Understanding Breastfeeding Video Program
 Debbie Young, MSL, ICCE, LCCE, CLC, ICBD, is the Customer Relations Manager at InJoy. Working with families as an educator and doula for over 30 years and after using InJoy products in her work since 1994, Debbie joined the InJoy team in 2013. She continues to be involved with families as a doula and a childbirth educator on a part-time basis. She teaches, writes and speaks on various birth, postpartum and building family subjects. Debbie is a past president of DONA International and was the Managing Editor for the International Doula for eight years. She is the current President of ICEA. She has a BA in Health Promotion: Women’s Health and a Master’s in Leadership through Grand Canyon University. Debbie has interviewed many leading professionals in the Maternal/Child field.
Debbie Young, MSL, ICCE, LCCE, CLC, ICBD, is the Customer Relations Manager at InJoy. Working with families as an educator and doula for over 30 years and after using InJoy products in her work since 1994, Debbie joined the InJoy team in 2013. She continues to be involved with families as a doula and a childbirth educator on a part-time basis. She teaches, writes and speaks on various birth, postpartum and building family subjects. Debbie is a past president of DONA International and was the Managing Editor for the International Doula for eight years. She is the current President of ICEA. She has a BA in Health Promotion: Women’s Health and a Master’s in Leadership through Grand Canyon University. Debbie has interviewed many leading professionals in the Maternal/Child field.











